DR KIM LINTON - REFRACT STUDY, CHRISTIE HOSPITAL
I’ve just had my sixth treatment on the Bispecifics trial, with six more to go of the weekly injections and then it switches to monthly for a further nine. Everything has gone smoothly so far; long may that continue. I still can’t quite believe my luck at randomising to Epcoritamab, the future would’ve looked very much bleaker otherwise. I can’t imagine a better Christmas present than this, it really is incredible.
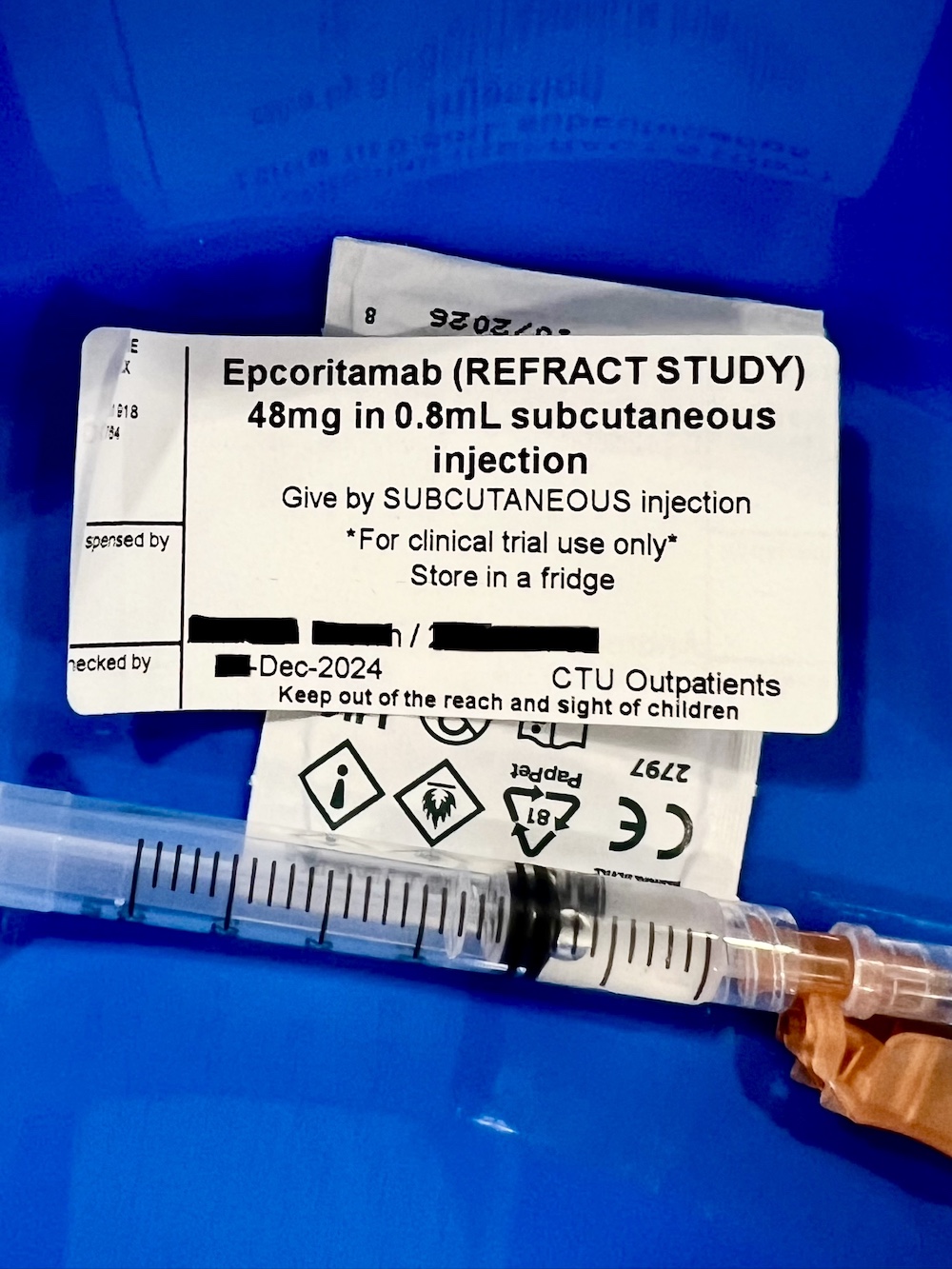
The first three weeks are ‘starter’ doses of Epcoritamab, circa 1mg, 2mg and 3mg. Week four is the first full dose when it jumps to 48mg. The low initial doses to make sure there are no adverse reactions. The steroid Dexamethasone is also given for the first four weeks as supportive treatment for any immune system reaction and to reduce significantly the size of the diseased nodes.
Week five and thereafter continues at the 48mg maximum dose but without the steroids. It’s then down to the combination of the Epcoritamab and Lenalidomide to tackle the cancer. (The Lenalidomide is a 28-day cycle, a daily pill for 21 days then 7 days off.)
The main adverse reaction risk with Epcoritamab is CRS, Cytokine Release Syndrome, causing fever, and also ICANS, a neurological disorder related to CRS. We have to watch for high temperature and any signs of confusion, Jo wanted to know how that was different from normal confusion …
Dr Kim Linton co-leads the Medical Oncology Lymphoma team at the Christie and is also a Senior Lecturer and Honorary Consultant in Lymphoma at the University of Manchester. Everyone I’ve met on the lymphoma team so far has been really impressive, I’m now ten years since diagnosis and after three relapses I really need to be at a specialist centre like this.
My follicular lymphoma is now ‘Relapsed/Refractory’, which I understand accounts for about 20% of FL patients. These are the difficult to treat cases unfortunately, with the disease coming back relatively quickly after treatment or not even responding to some treatments. In my case I’ve needed treatment every two to three years, whereas many FL patients have much longer remissions. A study by the Huntsman Cancer Institute comparing Bendamustine versus RCHOP chemo regimes for over 2k patients found the average time for further treatment was 8 years for Bendamustine and 6.5 years for RCHOP. I can only dream of remission periods like that!
This is why I need an alternative to chemotherapy. Immunotherapy has to be the future for lymphoma treatment. If I had Bendamustine chemo then I guess that would get me another couple of years, so will Epcoritamab get me any longer? That’s assuming the treatment works of course. That’s what I’m going to be finding out.
For those of us with relapsed/refractory FL, the other key factor is the number of treatments available. If you relapse every couple of years there need to be plenty of options. Bendamustine is the only standard chemo I haven’t had, so Bispecifics and CAR-T are vital to add to the list.